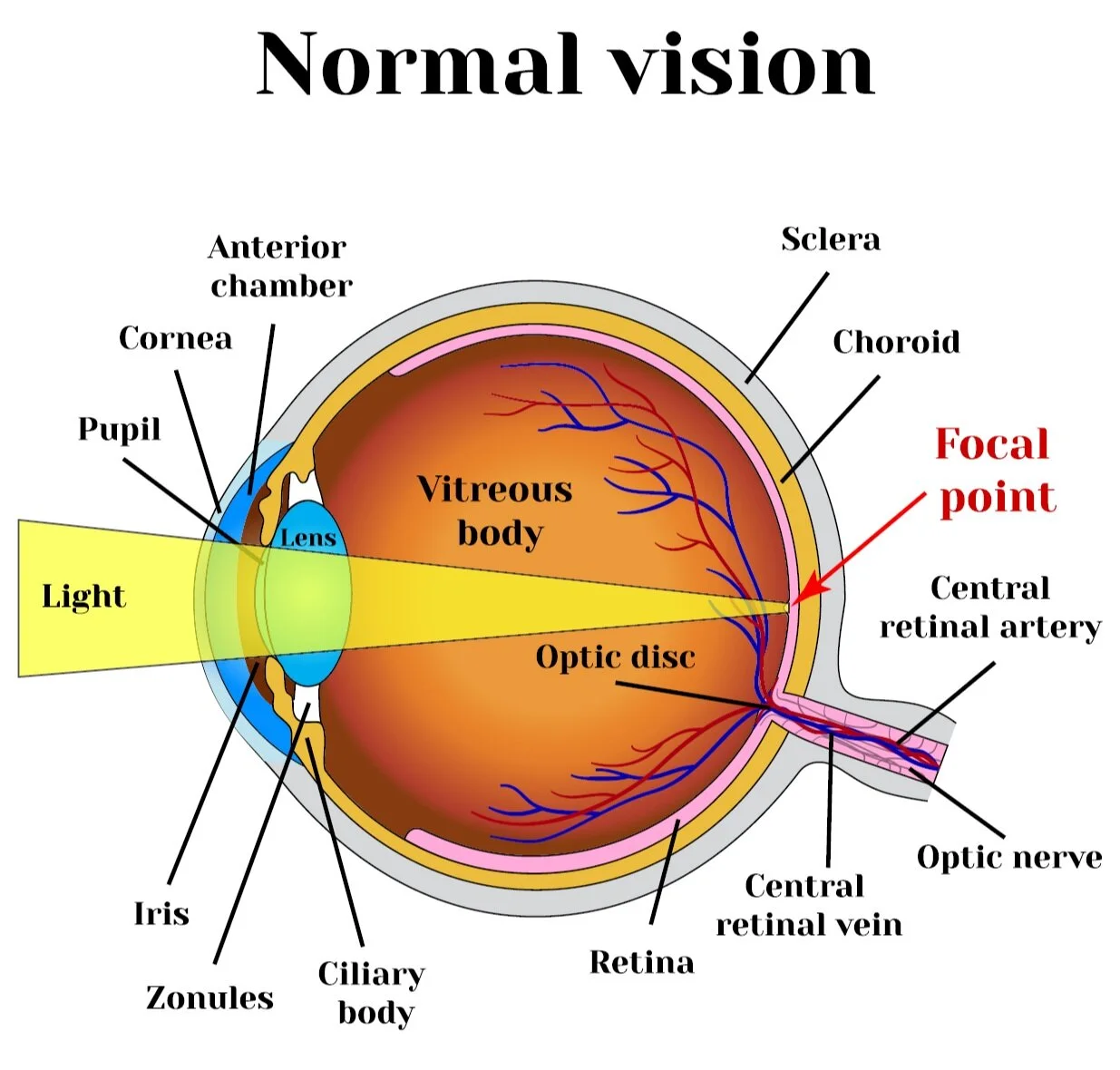
Structure of the Eye & Function
Cornea
Transparent part of the the eye that acts as a lens refracting 2/3rds of the total power of the eye. Light enters through the 5 layers of the cornea. Approximately 43 diopters of power is refracted.
Epithelium
Bowmans
Stroma (90% of Corneal thickness)
Descemets
Endothelium (regulates fluid transfer)
6th Layer (Dua’s Layer)
Notes:
Prefix = Kerat (As in Keratometer, or Kerataconus).
Does not have or need blood vessels. From the outside the cornea derives oxygen from tears through diffusion and from the inside via the aqueous humor.
Diameter: 11.5 mm
CT: 0.5 - 06 mms
ET: 0.6 - 0.8 mms
Refractive Index: 1.376
Positive Meniscus Lens: <
Pupil
After passing through the cornea and the aqueous humor, light enters through the pupil. The pupil is an opening (dark part) of the eye. Dilation of the pupil makes the opening bigger and allows more light into the eyes. The iris (contractile rings) controls the size of the pupil.
Notes:
Gets Wider in the Dark (3-8 mms)
and Narrower in the Light (2-4 )
Miosis (Constriction of the pupil)
Mydriasis (Dilation of the pupil)
PERRLA: An examination of pupilary function includes inspecting the pupils for equal size (1 mm or less of difference may be normal), regular shape, reactivity to light, and direct and consensual accommodation. These steps can be easily remembered with the mnemonic PERRLA (D+C): Pupils Equal and Round; Reactive to Light and Accommodation (Direct and Consensual).
CRYSTALLINE Lens
The Lens of the eye changes shape to refract light onto the retina. The lens works in conjunction with the cornea but the change in shape allows us to focus at objects at different distances. It is a biconvex shape ().
Notes:
The change in shape is know as accommodation. At short distances the ciliary muscles contract causing the zonule fibers to loosen, the lens thickens (becomes more round)
Roughly 10 mm in height and 4 mm thick but the shape/size can change due to accommodation.
The lens does not have nerves, blood supply, or connective tissue.
Roughly 18 dioptres of power. The shape is controlled by the ciliary muscles and is part of the UVEA.
Blocks UV rays in the range of 300-400 nm, the cornea blocks shorter UV ranges.
IOR - 1.42
Iris
PLR (Pupillary Light Reflex) controls the amount of light that enters the eyes by regulating the diameter of the pupil. Two groups of muscles;
Sphicnter Pupillae
Dilator Pupillae
Notes:
Iris + Ciliary Body + Choroid = UVEA
Ciliary Body
Part of the eye that contains the Ciliary muscle & the ciliary epithelium. The ciliary muscle controls the shape of the lens and the ciliary epithelium produces aqueous humor. The ciliary body is attached to the lens by zonular fibers or “Fibers of Zinn”. When these fibers are relaxed the lens changes shape and focuses light onto the retina.
Notes:
3 Main Functions: Accommodation, produce and absorb aqueous humor, and providing support to the zonular fibers which in turn provides support for the lens.
Zonules
A zonule or “little band” are part of the UVEA. The zonules of zinn connect the ciliary body and the lens of the eye.
Anterior Chamber
Anterior Chamber - EZ
Located between the Iris & the Cornea, this chamber is filled with aqueous humor.
Depth: 1.5 mm to 4.0 mm (average 3.0 mm) Depth lower than 2.5 mm increases risk factors to closed angle glaucoma. The “EZ (E=distance between limbus and center of pupil, Z = distance between limbus and cornea) method estimates the thickness of the anterior chamber.
Vitreous Body
A clear gel inside the eye that is located between the retina and the lens. The vitreous humor protects and maintains the shape of the eye. Light passes through this clear fluid onto the retina.
Notes:
4/5th the total volume of the eye, 99.5% of the fluid is made up of water.
Refractive index of 1.336
Vitreous means “glass” in Latin.
The Vitreous Humor cannot regenerate.
Optic Disc
Also known as the “Optic Nerve Head” is a blind spot in the eye that has no rods or cones. The Optic Disc is the exit point for neurons called RGC (retinal ganglion cell). These cells form the optic nerve, and the optic disc is the beginning of the optic nerve. The depression in the optic disc is called the “optic cup”. The ratio off these two areas are used to help diagnose glaucoma and is known as C/D ratios (cup to disc rations)
Notes:
Can be seen through retinal imaging.
C/D Ratio (Cup to Disc) is usually between 0.4 - 0.7 and higher ratios may be a sign of glaucoma (further testing would be needed as some patients are born with higher ratios). The 0.4 means that 4/10th of the cup covers the disc.
Optic Nerve
Transmits visual information from the Retina to the brain. Located at the back of the eye and near the ANNULES of ZINN.
Retina
Light converges or is refracted onto the retina and this visual information is transmitted through the optic nerve to the brain. Information is received on photoreceptor cells (rods or cones). The macula is found in the center of the retina.
Macula
Located in the center of the retina and responsible for high acuity vision or seeing fine details. Contains rods and cones which are photoreceptors of the eye and is the central portion of the retina. The central fovea (small pit) is densely populated by cones.
Notes:
Diameter about 5.5 mm (fovea 1.5 mm).
The macula’s natural yellow color works as a UV blocker absorbing most of the blue and ultraviolet light.
Damage to the Macula will result in loss of central vision.
Sclera
The sclera maintains the shape of the eye and also serves as the attachment for the muscles that control eye movement. It is the “white” portion of the eyeball composed of flexible collagen fibers.
Notes:
In children the sclera is slightly blue
Rods
Photoreceptor cell that is mainly responsible for peripheral vision, night vision (less intense light), and has little assistance with color vision. This is why color is not apparent in lower light settings. Usually located in the outer edges of the retina.
Notes:
92 million rods in human body
Cones
Photoreceptor cells that are mainly responsible for fine details and color. Work best in bright light settings and mostly located in the fovea centralis.
Notes:
6-7 million cones in the human body.
3 Types - S (short), M (Medium), & L (Long) Wavelength Cones
Choroid
Located between the sclera and the retina this is the vascular layer of the eye. It’s primary function is to provide nourishment and oxygen to the retina.
Notes:
4 layers:
Hallers (large blood vessels), Sattlers (medium blood vessels), Choriocapillaris (layer of capillaries), Bruch’s membrance (innermost layer, transports wastes from photoreceptors to the choroid).
Works like a spring, when the ciliary muscles are relaxed the choroid pulls on the lens of the eye making it flat. When the muscles are contracted the zonules relax causing the lens of the eye to thicken (becomes more plus).
Rear portion of the eye is the thickest 2mm, compared to 1mm near the front.
Melanin in the choroid reduces reflections within the eye.
Central Retinal Vein
Drains blood through the optic nerve from retinal capillaries into the cavernous sinus.
Central Retinal Artery
Runs below the optic nerve and enters the eye close to the nerve. Provides blood supply to the retina through terminal branches.
Limbus
Border between the cornea and the sclera.
Conjunctiva
Keeps the eyes lubricated and moist which allows the eyes to move without friction or irritation. The conjunctiva is a clear membrane that covers a portion of the sclera and is behind the eyelids. It does not cover the cornea and has two parts the bulbar conjunctiva and the palpebral (or tarsal) conjunctiva. The palpebral conjunctiva lines the posterior portion of the eyelids while the bulbar conjunctiva lines the anterior portion of the sclera. The point where these two parts meet is called the Fornix conjunctiva. The conjunctiva protects our eyes from debris and helps prevents infections from microorganisms.
Tenon’s Capsule
Also “fascia bulbi”, covers the eyeball from the optic nerve to the limbus. Smooth inner surface that separates the the eye from the orbital fat and allows movement.
Eye Muscles and Movement
There are 6 muscles that control eye movement. When these muscles contract they pull the eye toward that muscle. The 4 Rectus muscles originate from the ANNULES of ZINN. The rectus muslces work against each other and control eye movement in the cardinal directions.
The oblique muscles attach at angles on the eyeball and control the rotation of the eye. The oblique muscles assist the rectus muscles in their movements.
Lateral Rectus Muscle:
Horizontally moves eye away from nose (also known as abduction).
(outward away from nasal)
Medial Rectus Muscle:
Muscle that is closest to the nose (or in the middle). Assists with moving the eye up & down as well as from side to side. Helps keep the pupil in place and when there are issues with this muscle and the two pupils are misaligned the condition is called Strabismus.
(inward toward nasal)
Inferior Rectus Muscle:
Moves the eye downward and inward towards the nose. It is the only muscle that can depress the pupil when it is fully abducted (raised).
(downward & slightly inward)
Superior Rectus Muscle:
Works in conjunction with the inferior oblique muscle to move the eye upward.
(upward & slightly outward)
Inferior Oblique:
Only muscles that does not originate from the ANNULES of ZINN. Originates from the orbital surface of maxilla. It is partially covered by the inferior rectus muscle.
Rotation of the eye outwards (extorsion)
Movement of the eye upwards (movement superior or elevation)
Movement of the eye laterally away from the nose (abduction)
(outward & upward)
Superior Oblique:
Rotate the eye and work along with the rectus muscles to control movement.
(outward & downward)
Lacrimal System
The Lacrimal system include the lacrimal gland, the lacrimal ducts (canals), lacrimal sac,
Lacrimal Glands
Tear producing glands that produce the aqueous layer of the tear film. Inflammation of this area is call dacryoadentitis
Lacrimal Ducts
Consists of the Superior Duct (shorter) and the Inferior Duct which transmit tears from the eye to the lacrimal sac.
Lacrimal Sac
Reservoir for the overflow of tears received from the lacrimal ducts.
Eyelids
a = lacrimal gland
b = superior lacrimal punctum
c = superior lacrimal canal
d = lacrimal sac
e = inferior lacrimal punctum
f = inferior lacrimal canal
g = nasolacrimal canal
Meibomian Glands (tarsal glands) secrets an oily substance called meibum that prevents tears from evaporation. There are 50 glands on the upper eyelid and 25 on the lower.
Lacrimal glands are almond shaped exocrine glands that secrete the aqueous layer of the tear film. The tears go to the lacrimal sac (reservoir for overflow of tears) and then drain out of the lacrimal duct and into the nose.